When we talk about giving medicine, there are a few important ideas that come up, particularly for those working as nurses. It's really about making sure the right amount of a substance gets to someone at the right moment. This attention to detail, you know, it's pretty central to looking after people, especially in sensitive areas like caring for new mothers and their babies.
The words "dose" and "dosage" often get used, and sometimes they seem to mean the same thing, but they actually point to different parts of the medicine-giving process. One word talks about a single amount, while the other brings in the idea of time and how often that amount should be given. For nurses, particularly those who help with maternal newborn care, getting these ideas straight is, like, absolutely vital for providing good support.
Thinking about something like a proctored assessment, especially one focused on dosage calculation for RNs in maternal newborn settings, it becomes clear just how much these basic definitions matter. It's not just about memorizing facts; it's about having a solid grasp of how these concepts play out in real situations. The goal is, you know, always to help patients get better with as few problems as possible, and that begins with understanding the medicine itself.
Table of Contents
- What is a Drug Dose in Maternal Newborn Care?
- How does Dosage differ from Dose in Maternal Newborn Practice?
- Why is Accurate Dosage Calculation Important for RNs?
- What Challenges Might RNs Face with Dosage Calculation in Maternal Newborn Settings?
- Considering the Maternal Newborn Proctored Assessment 3.2 - What Does It Cover?
- How Can Understanding Dosage Calculation Aid RNs in Maternal Newborn Scenarios?
- What Role Does Precision Play in Dosage Calculation for Maternal Newborn RNs?
- Looking at the Bigger Picture of Dosage Calculation for RNs
What is a Drug Dose in Maternal Newborn Care?
Let's get down to what a "dose" truly means. Simply put, a drug dose is a specific amount or, perhaps, a certain weight of medicine. It's that single, measured portion of a substance given at one particular time. For example, when someone says, "Take one pill," that one pill represents a dose. It's the individual quantity of a medicine that a person receives on a single occasion. This idea of a distinct amount is, like, very important in all areas of medicine, including the sensitive field of maternal newborn care.
Picture it this way: a dose is the precise quantity of a healing substance that is put into a patient's body in one go. It’s a fixed measure, whether it's a liquid, a tablet, or something else entirely. This exact quantity is determined by many factors, but at its core, it's about that one-time delivery of the therapeutic agent. So, it's almost like a single serving of medication, you know?
In the context of looking after new mothers and their little ones, knowing the exact amount of a dose is absolutely fundamental. Whether it's a medicine for pain relief for a mother after childbirth or a tiny bit of something to help a newborn, the specific quantity given at one moment is what we call a dose. It's a foundational piece of information that healthcare providers, especially those with RN responsibilities in maternal newborn settings, rely on every single day. This concept forms a very basic building block for all subsequent calculations and administration schedules.
- Bars Royersford
- Northwoods Falconry
- Secret Recipes Family Dining Photos
- Family Friendly Fans
- Champion Car Wash
We often hear medical professionals use this word, "dose," when they are talking about how much of a medicine to take right now. It's the instant measurement, the quantity that is given without reference to how often it will be given again. It’s the immediate "how much" part of the instruction. So, if you are thinking about, say, a particular antibiotic, the dose would be the specific milligram amount of that medicine given at one point in time, that is pretty much it.
How does Dosage differ from Dose in Maternal Newborn Practice?
Now, if a dose is that single, specific amount, what then is "dosage"? Well, dosage takes that single amount and adds the element of time to it. It's not just about how much, but also about how often and for how long that medicine should be given. So, a dosage refers to the duration or the frequency at which a medicine must be taken or administered. It's the whole plan for giving the medicine, rather than just one part of it. This distinction is, you know, very important for RNs working in maternal newborn care.
When we consider the broader picture of pharmacology and medicine, dosage points to the entire prescribed way of giving a medicine or substance. This includes the amount of each dose, how often those doses should be given, and for what length of time the treatment should continue. It’s the predetermined amount and rate of administration of a medicine for a patient, as set out by a medical expert. So, while a dose is a specific quantity given at one time, dosage brings in the rhythm and regularity of those quantities over a period. It's a bit like the entire schedule for taking a medicine, actually.
The American Medical Association, for instance, has its own way of defining dosage, reinforcing that it's more than just a single amount. It’s the full set of instructions for how a medicine should be used to get the best effect with the fewest unwanted reactions. This means considering the optimal dosage, which is the amount and schedule that gives the desired outcome while keeping side effects to a minimum. For RNs, particularly those involved in maternal newborn health, grasping this full picture of dosage is, you know, absolutely critical for safe and effective care.
To illustrate, if a dose is, say, 250 milligrams of a particular medicine, the dosage might be "250 milligrams every six hours for ten days." That "every six hours for ten days" part is what makes it a dosage, adding the time element to the amount. It’s the complete regimen, the full set of instructions for administering the substance. This detailed plan helps ensure that the medicine works as intended and that the patient receives consistent care, which is, like, pretty important for patient well-being, especially with a maternal newborn proctored assessment.
Why is Accurate Dosage Calculation Important for RNs?
Why does getting these numbers just right matter so much for nurses, especially for those who provide care to new mothers and babies? Well, the simple truth is that giving the wrong amount of medicine, or giving it at the wrong time, can have serious, serious consequences. For patients who are already vulnerable, like a new mother recovering from childbirth or a tiny newborn, even a small mistake can lead to big problems. So, it's a matter of patient safety, pure and simple, you know?
Accurate dosage calculation for RNs is a foundational skill because it directly impacts patient outcomes. It’s about making sure the patient gets exactly what they need, no more and no less. If a dose is too small, the medicine might not work, leaving the patient unwell. If it’s too large, it could cause harmful side effects, or even be life-threatening. This precision is, like, absolutely vital in every medical setting, but perhaps even more so when dealing with the delicate physiology of mothers and their infants.
The body systems of newborns, for example, are still developing, which means they process medicines differently than adults. This makes the exact calculation of a dose, and the proper schedule of its dosage, incredibly important. A nurse’s ability to perform these calculations correctly is a key part of their professional competence and a cornerstone of safe patient care. It's a skill that, you know, really shows a nurse's dedication to their patients' well-being.
Consider the trust that patients and their families place in healthcare professionals. They expect that the care provided will be of the highest standard, and that includes the safe administration of medicines. Accurate dosage calculation for RNs upholds this trust and helps prevent errors that could lead to harm. It’s a direct reflection of a nurse’s commitment to doing what is right for every single person under their care, which is, like, a pretty big responsibility, obviously.
What Challenges Might RNs Face with Dosage Calculation in Maternal Newborn Settings?
Even with a clear grasp of what dose and dosage mean, nurses can still run into difficulties when it comes to figuring out the right amounts of medicine. One challenge, for instance, is that patients in maternal newborn settings often have unique needs. A mother might have different requirements than her baby, and even among babies, their size and age can vary significantly, which impacts how much medicine they need. So, there's a lot of individual variation to consider, you know?
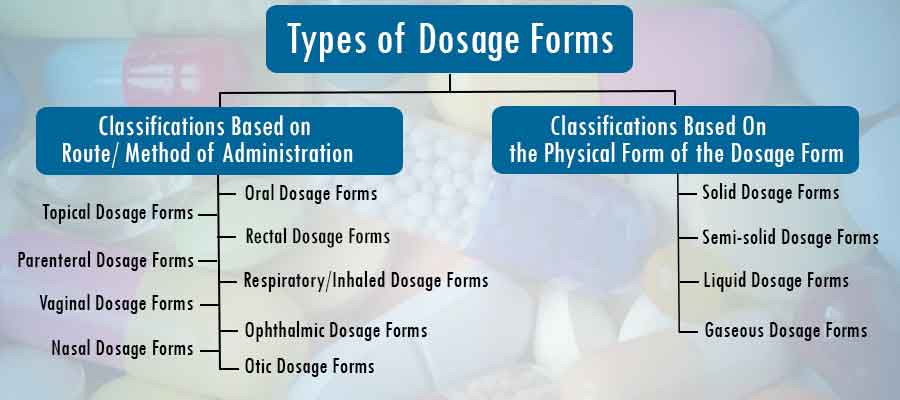
Another point of difficulty can be the sheer variety of medicines and their different forms. Some might come in liquid form, others as pills, and some might need to be given through an IV. Each form might require a different way of calculating the dose, adding layers of complexity to the task. The nurse must be able to switch between these different calculation methods smoothly and accurately, which can be, like, quite a mental exercise.
Then there’s the pressure of the clinical environment itself. Nurses often work in busy places, with many demands on their attention. Distractions, time constraints, and the need to act quickly can all add to the difficulty of performing dosage calculation for RNs without error. It takes a calm head and a methodical approach to ensure that every calculation is checked and double-checked, even when things are moving fast. It's a very demanding aspect of the job, really.
Furthermore, some medicines used in maternal newborn care might be what we call "high-alert" medications, meaning a small mistake could have a very serious outcome. These medicines demand an even higher level of caution and precision in their calculation and administration. The stakes are, like, incredibly high, which means the nurse must be absolutely confident in their mathematical abilities and their understanding of how these medicines work. It’s a constant need for vigilance and accuracy in dosage calculation for RNs in maternal newborn settings.
Considering the Maternal Newborn Proctored Assessment 3.2 - What Does It Cover?
While I cannot tell you the specific content of any particular assessment, we can talk about why an assessment like the "maternal newborn proctored assessment 3.2" would place a strong focus on dosage calculation for RNs. Such an evaluation would likely aim to ensure that a nurse has a firm grip on the principles of safe medication administration within this specialized area. It’s about confirming that a nurse can take what they know about doses and dosages and apply it in situations relevant to mothers and their babies. So, it's more about demonstrating practical application, you know?
The very nature of a proctored assessment suggests a formal test of a nurse’s knowledge and skills. In the context of maternal newborn care, this would mean evaluating their capacity to work with the specific types of medicines and patient populations found there. It’s about ensuring that a nurse is prepared to handle the unique considerations that come with caring for pregnant individuals, new mothers, and infants, where medication needs can be quite different from other patient groups. This kind of assessment is, like, a way to verify readiness for real-world scenarios.
Any assessment involving dosage calculation for RNs would naturally test a nurse’s ability to interpret a prescription, convert units of measurement, and arrive at the correct amount of medicine to give. It would also likely assess their understanding of the difference between a single dose and a full dosage regimen. The goal is to see if the nurse can perform these essential tasks accurately and reliably, which is, you know, a pretty big deal for patient safety in maternal newborn care.
The number "3.2" in the assessment title might suggest it’s part of a series or a particular version, perhaps building on previous knowledge or focusing on specific aspects of care. Regardless of the exact content, the core idea remains the same: proving competence in a skill that is absolutely central to nursing practice. It’s about showing that a nurse can handle the responsibility of medication administration with precision and care, especially in the sensitive environment of maternal newborn care. This kind of test, you know, really helps ensure high standards.
How Can Understanding Dosage Calculation Aid RNs in Maternal Newborn Scenarios?
Having a solid grasp of dosage calculation for RNs can provide a nurse with a great deal of confidence when working with mothers and newborns. When you truly understand the difference between a dose and a dosage, and how to figure out the right amounts, it reduces the chance of making errors. This confidence allows a nurse to focus more on the patient’s needs and less on worrying about the math, which is, like, pretty helpful in a busy setting.
Knowing how to calculate medicine amounts accurately also means a nurse can better advocate for their patients. If something on a prescription looks off, or if a patient’s condition changes in a way that might affect their medicine needs, a nurse with strong calculation skills can spot potential problems and raise concerns. This proactive approach helps keep patients safe and ensures they receive the most appropriate care, which is, you know, a very important part of being an RN in maternal newborn care.
Furthermore, a deep understanding of dosage calculation for RNs helps in educating patients and their families. Nurses often explain how much medicine to take, how often, and for how long. When a nurse is clear and confident in these instructions, it helps patients and their caregivers follow the plan correctly, leading to better health outcomes. It’s about empowering families with the right information, basically.
Ultimately, proficiency in dosage calculation for RNs contributes to a higher quality of care overall. It’s a fundamental skill that underpins safe practice in every aspect of nursing, but particularly where the patients are so delicate and sensitive to medication, as is the case in maternal newborn settings. It truly helps nurses provide the best possible support to those who are bringing new life into the world and starting their family journey, which is, like, a pretty amazing thing to be a part of.
What Role Does Precision Play in Dosage Calculation for Maternal Newborn RNs?
Precision, or getting things exactly right, is absolutely key when it comes to dosage calculation for RNs, especially in the maternal newborn field. For tiny babies, even a very small difference in a dose can have a huge impact because their bodies are so small and still developing. Their systems might not be able to handle amounts that would be perfectly fine for an adult. So, every single drop and every single milligram matters, you know?
Consider how medicines are often given to newborns based on their weight. This means a calculation must be done for each individual baby, and that calculation needs to be spot-on. There’s very little room for error when you are working with such small numbers and such delicate patients. This need for exactness is what makes the role of precision in dosage calculation for maternal newborn RNs so incredibly important.
For mothers, too, precision in dosage calculation for RNs is vital. Whether it’s a medicine to manage pain after delivery or something to help with a specific health condition, the exact amount and timing can affect their recovery and well-being. An incorrect dose could slow down their healing or cause unwanted side effects, which is, like, something we want to avoid at all costs.
The importance of precision also extends to the timing of medicine administration. Dosage, as we discussed, involves frequency. Giving a medicine too early or too late can also affect how well it works and whether it causes problems. So, it’s not just about the amount, but also about the schedule being followed with great exactness. This meticulous attention to detail is, like, a hallmark of excellent nursing care in maternal newborn settings.
Looking at the Bigger Picture of Dosage Calculation for RNs
When we step back and look at the whole idea of dosage calculation for RNs, it’s clear that it’s more than just a math problem. It’s a core component of patient safety and a reflection of a nurse’s professional responsibility. Every time a nurse prepares or administers medicine, they are making a decision that directly affects someone’s health, sometimes even their life. So, it’s a very serious undertaking, you know?
The distinction between a "dose" and a "dosage" is fundamental to this entire process. One is the specific quantity given at one time, and the other is the complete plan for how that quantity, or quantities, will be given over a period. Understanding both of these ideas, and how they fit together, is absolutely essential for any nurse, particularly those working in specialized fields like maternal newborn care. It's, like, the very foundation of giving medicine safely.
The challenges that come with dosage calculation for RNs are real, from the unique needs of patients in maternal newborn settings to the pressures of the clinical environment. However, with a solid grasp of the basics and a commitment to precision, nurses can overcome these hurdles. Their ability to perform these calculations accurately directly contributes to the well-being of new mothers and their precious babies. It’s a skill that truly makes a difference, basically.
So, whether it’s for a proctored assessment or for daily practice, the importance of mastering dosage calculation for RNs cannot be overstated. It’s a skill that empowers nurses to provide the highest standard of care, ensuring that every patient receives the right medicine, in the right amount, at the right time. This focus on accuracy and patient safety is, like, at the very heart of what it means to be a compassionate and effective healthcare provider in the maternal newborn field.